Achilles Tendonitis
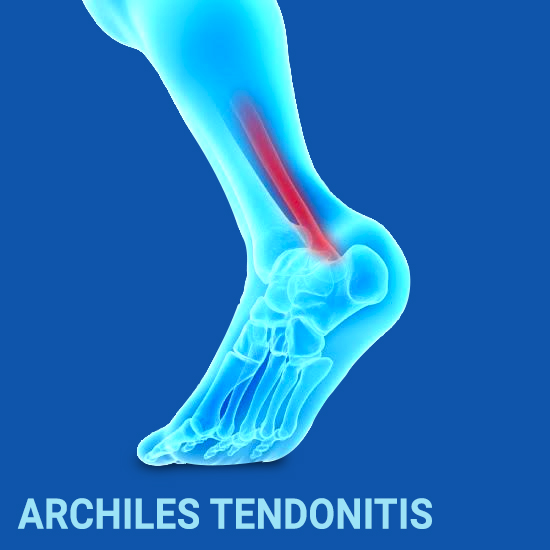 The Achilles tendon is the largest tendon in the human body that attaches the calf muscles to the heel bone of the foot. Achilles Tendon enables walking by helping to raise the heel off the ground. You put Achilles Tendon to use when you walk, jump, run and push up on your toes. Overuse of Achilles Tendon results in Achilles Tendonitis, an inflammation in the tendon. Anyone whose work puts stress on their ankles and feet is more susceptible to Achilles Tendonitis. Athletes are at high risk – those who participate in athletics only on weekends or infrequently. Those who are less conditionedfor intensive physical activity, age, people with excessive pronation are also more susceptible to develop Achilles Tendonitis.
The Achilles tendon is the largest tendon in the human body that attaches the calf muscles to the heel bone of the foot. Achilles Tendon enables walking by helping to raise the heel off the ground. You put Achilles Tendon to use when you walk, jump, run and push up on your toes. Overuse of Achilles Tendon results in Achilles Tendonitis, an inflammation in the tendon. Anyone whose work puts stress on their ankles and feet is more susceptible to Achilles Tendonitis. Athletes are at high risk – those who participate in athletics only on weekends or infrequently. Those who are less conditionedfor intensive physical activity, age, people with excessive pronation are also more susceptible to develop Achilles Tendonitis.
Depending upon the location of inflammation there are two types of Achilles Tendonitis, namely,
Insertional Achilles Tendinitis – the lower portion of the tendon where it attaches to the heel bone gets affected
Noninsertional Achilles tendonitis – fibres in the middle portion of the tendon gets affected
Achilles Tendonitis is short-lived. Usually, simple home treatment will help you recover from the condition. However, if left unchecked, Achilles Tendonitis will further progress into a tendon tear or rupture associated with continued pain which might need medication or surgery.
Causes
Achilles Tendonitis is nothing but an overuse disorder. The sudden increase of repetitive activity too quickly involving the Achilles Tendon leads to injury of tendon fibres due to too much stress caused. The ongoing stress will hinder the repair of the injured tissue and will alter the structure of the tendon fibre resulting in continued pain.
Some of the common causes which can potentially cause Achilles Tendonitis include
- A sudden increase in physical activity
- Poorly fitting footwear/shoes
- Exercising without doing warm-up
- Continuously straining the calf muscles during repeated exercise or intense physical activity
- Wearing high heels every day or prolonged use
- Sports that demands abrupts transition such as Tennis, Football, Running, Gymnastics, Basketball.
- Flat feet (fallen arches)
- Tight leg muscles or tendons
- Leg Length Discrepancy
- Cold weather training
- The bony growth on the back of the ankle – bone spur
- Fluoroquinolones, a class of antibiotic drug, has been linked to Achilles Tendonitis, in rare cases
- Medical condition such as psoriasis, high blood pressure
- Age, the Achilles Tendon weakens as you age
Symptoms
Begins with painusually a mild ache or burning sensation in the back of the leg or above the heel that worsens with physical activity. Swelling at the backside of your heel that is present all the time and gets worse with activity. Also,
- Pain that worsens with activity
- Tenderness or stiffness in the morning
- Limited movement when you flex your foot
- Tight calf muscles
- The skin on your heel overly warm to touch
- Pain above your heel when you try to stretch your ankle or try to stand on your toes
- If the condition worsens you may have trouble pointing your toes or difficulty in pushing off your toes when you take a step
- When the tendon ruptures you may hear a pop or snap along with severe heel pain and a visible gap where the tendon ruptured
Diagnosis
The doctor will clinically examine the patient’s ankle and foot to evaluate the range of motion to determine the condition of the tendon. Imaging modalities such as X-ray, MRI scan, Ultrasounds are also helpful in the evaluation of Achilles Tendonitis. Sometimes the doctor may go for a blood test to check for inflammation.
Treatment
Rest–Reduce or stop physical activity. Avoid putting weight on your leg. Switch to low impact activities if you want to remain active.
Ice–Applyice bag wrapped in a towel to reduce swelling and pain. Do not apply ice directly against the skin.
Elevation–Raise your leg using a pillow to reduce swelling while sitting or lying down
Oral medications–Anti-inflammatory medication such as ibuprofen and naproxen will help with swelling and pain
Orthotics–Custom orthotic devices, especially, for those with overpronation may require to protect the Achilles Tendon from further stretching.
Night Splints–Wear a night splint/brace to hold the foot with the toes pointed up to maintain a stretch in Achilles Tendon during sleep.
Surgery–When non-surgical treatment approaches fail, surgery may be required to restore the Achilles tendon.
Recovery
Recovery depends upon the severity of injury/inflammation. It may take months to heal completely. Stretching and strengthening exercise as advised by the healthcare provider can help prevent further damage to Achilles tendon and will speed up the healing process.
Prevention.
After the treatment, increase your activity level gradually. Warm-up before strenuous activity. Limit or avoid physical activities that put excessive stress on the Achilles Tendons. Daily exercise especially stretching and strengthening of calf muscles, after the treatment of Achilles Tendonitis is recommended. Prevent the recurrence of Achilles Tendonitis by wearing proper-fitting shoes according to your foot type and activity involved.
